Main Body
Module 3 What are the Effects of Chromosomes and Hormones on Gender?
Case Study: Pidgeon Pagonis
Pidgeon Pagonis, an intersex activist, was born in Chicago in 1986 and declared female at birth. At three months of age, their (preferred pronoun) mother was concerned that Pidgeon’s genitals looked swollen. Tests indicated that Pidgeon was genetically male with XY chromosomes and internal testes. Doctors at the time recommended that Pidgeon receive surgery to appear fully female. Further, doctors told Pidgeon’s parents that the surgery would not harm them sexually and it would allow them to have a “normal life” as a female. Consequently, Pidgeon had two surgeries at the ages of 4 and 11. However, according to Pidgeon the surgeries resulted in “scarring, loss of sensation, emotional trauma, and severe sexual impairment” (Schoenberg, 2018, p. 1).
Attempting to normalize external genitalia through surgery has typically been recommended for children who display differences in sexual development, but many of the individuals who underwent this surgery identify significant negative experiences. Consequently, this standard procedure has recently been criticized by individuals with differences in sexual development who believe that they, and not doctors, should make decisions about whether to have surgery or not. According to Schoenberg (2018), The United Nations High Commissioner for Human Rights, former surgeon generals, and Human Rights Watch have all called for the end of these childhood surgeries. California became the first state to pass a resolution discouraging the surgeries. Pidgeon will continue to be active in the fight for stopping these purely cosmetic and unnecessary surgeries.
Heredity
As you learned in Introduction to Psychology, an individual’s development is affected by both nature and nurture. Nurture refers to all the environmental influences that affect an individual, and nurture influences will be discussed in future modules. Nature refers to the contribution of genetics to one’s development. The basic building block of the nature perspective is the gene. Genes are recipes for making proteins, while proteins influence the structure and functions of cells. Genes are located on the chromosomes, which are strands of DNA. There are an estimated 20,000-25,000 genes for humans, according to the Human Genome Project (NIH, 2020).
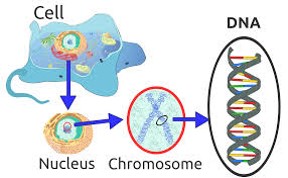
Normal human cells contain 46 chromosomes (or 23 pairs; one from each parent) in the nucleus of the cells. After conception, most cells of the body are created by a process called mitosis. Mitosis is defined as the cell’s nucleus making an exact copy of all the chromosomes and splitting into two new cells. However, the cells used in sexual reproduction, called the gametes (sperm or ova), are formed in a process called meiosis. In meiosis the gamete’s chromosomes duplicate, and then divide twice resulting in four cells containing only half the genetic material of the original gamete. Thus, each sperm and egg possesses only 23 chromosomes and combine to produce the normal 46.
Mitosis and Meiosis
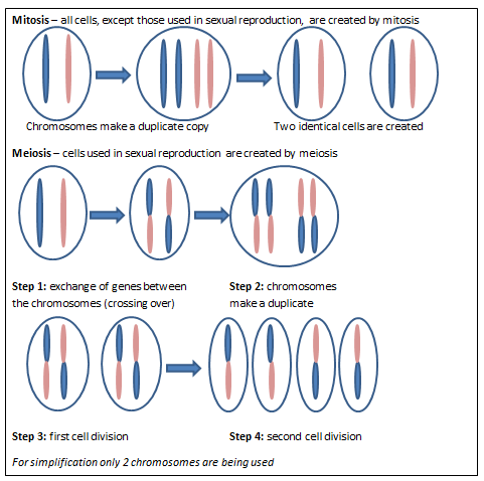
Of the 23 pairs of chromosomes created at conception, 22 pairs are similar in length. These are called autosomes. The remaining pair, or sex chromosomes, may differ in length. If a child receives the combination of XY the child will be identified as genetically male. If the child receives the combination XX the child will be identified as genetically female.
Genotypes and Phenotypes
The word genotype refers to the sum total of all the genes a person inherits. The word phenotype refers to the features that are actually expressed. Look in the mirror. What do you see, your genotype or your phenotype? What determines whether or not genes are expressed? Because genes are inherited in pairs on the chromosomes, we may receive either the same version of a gene from our mother and father, that is, be homozygous for that characteristic the gene influences. If we receive a different version of the gene from each parent, that is referred to as heterozygous. In the homozygous situation we will display that characteristic. It is in the heterozygous condition that it becomes clear that not all genes are created equal. Some genes are dominant, meaning they express themselves in the phenotype even when paired with a different version of the gene, while their silent partner is called recessive. Recessive genes express themselves only when paired with a similar version gene. Geneticists refer to different versions of a gene as alleles. Some dominant traits include having facial dimples, curly hair, normal vision, and dark hair. Some recessive traits include red hair, being nearsighted, and straight hair.
Most characteristics are not the result of a single gene; they are polygenic, meaning they are the result of several genes. In addition, the dominant and recessive patterns described above are usually not that simple either. Sometimes the dominant gene does not completely suppress the recessive gene; this is called incomplete dominance. An example of this can be found in the recessive gene disorder sickle cell disease. The gene that produces healthy round-shaped red blood cells is dominant. The recessive gene causes an abnormality in the shape of red blood cells; they take on a sickle form, which can clog the veins and deprive vital organs of oxygen and increase the risk of stroke. To inherit the disorder a person must receive the recessive gene from both parents. Those who have inherited only one recessive-gene are called carriers and should be unaffected by this recessive trait. Yet, carriers of sickle cell have some red blood cells that take on the c-shaped sickle pattern. Under circumstances of oxygen deprivation, such as high altitudes or physical exertion, carriers for the sickle cell gene may experience some of the symptoms of sickle cell disease (Berk, 2004).
Prenatal Exposure to Hormones
Just how important are genes and hormones to the development of gender identification? The answer is quite important, especially during the prenatal period. According to Hines (2011), “Growing evidence shows that prenatal exposure to the gonadal hormone, testosterone, contributes to the development of sex differences, including sexual orientation, core gender identity, and some sex-related cognitive and personality characteristics. In addition to these prenatal hormonal influences, early infancy and puberty may provide additional critical periods when hormones influence human neurobehavioral organization,” (p.69).
You might be surprised to learn that gender development occurs at the moment of conception. At that time either two X chromosomes or an X and a Y chromosome unite. This union is important in determining what the gonads, or reproductive organs, will become. This occurs during the fifth and sixth weeks of gestation. Two X chromosomes typically result in the development of ovaries, or the gonads that produce ova and ovarian hormones. An X and Y chromosome pattern typically results in the development of testes, or gonads inside the scrotum that produce sperm amd testosterone. The amount of testosterone produced is very different depending on the whether the embryo has an XX or XY pattern, and this difference appears to be at its maximum between weeks 8 and 24 prenatally (Hines, 2011).
Interestingly, at least 1 in every 1,000 conceptions results in a variation of chromosomal sex beyond the typical XX or XY sets. Some of these variations include, XXX, XXY, XYY, or even a single X (Dreger, 1998). In some cases, people may have unusual physical characteristics, such as being taller than average, having a thick neck, or being sterile (unable to reproduce), but in many cases, these individuals have no cognitive, physical, or sexual issues (Wisniewski et al, 2000).
Mullerian and Wolffian Ducts:
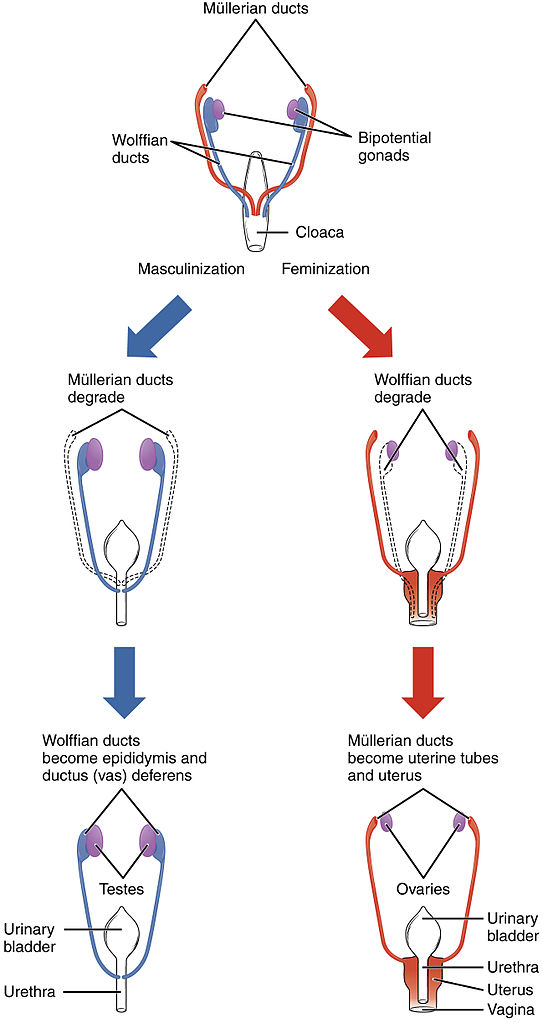
Until the seventh week, there is an innate tendency for all embryos to have female internal sex organs, unless there is the presence of the SRY gene, located on the Y-chromosome (Grumbach & Conte, 1998; Wizemann & Pardue, 2001). The SRY gene causes XY-embryos to develop the testes. The testes emit testosterone which stimulates the development of the Wolffian ducts, or primitive male internal sex organs. The Wolffian ducts then transform into the epididymis, seminal vesicles, and vas deferens. If the SRY gene is not present or active, which is typical for chromosomal females, then XX-embryos develop ovaries and the primitive female internal sex organs, or the Mullerian ducts, which transform into the fallopian tubes, uterus, cervix, and inner two-thirds of the vagina (Carlson, 1986). Without a burst of testosterone from the testes, the Wolffian ducts naturally deteriorate (Grumbach & Conte, 1998; Wizemann & Pardue, 2001). For XY-embryos, the testes also emit a Mullerian inhibiting substance, a hormone that causes the Mullerian ducts to atrophy. The concentration of androgens is especially high between weeks 8 and 24 (Hines, 2015).
By the 20th week of gestation, the external sex organs are fully formed. Formation of male external sex organs (e.g., the penis and scrotum) is dependent upon high levels of testosterone, whereas female external sex organs (e.g., the outer third of the vagina and the clitoris) form without hormonal influences (Carlson, 1986). When we think of identifying a newborn as a girl or boy, it is based on these external sex organs that are present at birth.
Because of the ethical concerns of manipulating gonadal hormones in humans, research done with nonhuman mammals provide hypotheses regarding the hormonal influences on brain development and behavior for humans. Specifically, estrogens during the early developmental period do not promote female typical behavior. Rather, female typical development occurs when there is an absence of male hormones (Hines, 2011). Consequently, high levels of estrogen do not feminize behavior. In contrast, the more testosterone an animal is exposed to, the more male typical behavior is demonstrated, such as rough and tumble play (Hines, 2015).
As described, levels of sex hormones, such as estrogen, testosterone, and progesterone, begin affecting the brain prenatally and are thought to impact future emotions, behaviors, and thoughts related to gender identity and sexual orientation (Swaab, 2004). However, it is important to understand that the interactions of chromosomes, gonads, hormones, internal sex organs, external sex organs, and brain differentiations during this developmental stage are too complex to readily conform to the familiar categories of sex, gender, and sexual orientation historically used to describe people (Herdt, 1996).
Differences in Sexual Development
The international scientific and medical communities, including the World Health Organization, World Medical Association, World Psychiatric Association, and Association for Psychological Science, view variations of sex, gender, and sexual orientation as normal. Furthermore, variations of sex, gender, and sexual orientation occur naturally throughout the animal kingdom. More than 65,000 animal species are intersex; that is born with either an absence or some combination of male and female reproductive organs, sex hormones, or sex chromosomes (Jarne & Auld, 2006). In humans, differences in sexual development make up more than 150 million people, or about two percent of the world’s population (Blackless et al., 2000). There are dozens of conditions, and such individuals demonstrate the diverse variations of biological sex. Some examples of differences in sexual development, include Turner syndrome, Triple X syndrome, Klinefelter’s syndrome, Jacob’s syndrome, Complete and Partial Androgen Insensitivity syndrome, and Congenital Adrenal Hyperplasia,. The term “syndrome” can be misleading; although such individuals may have physical limitations (e.g., about a third of Turner’s individuals have heart defects; Matura et al, 2007), they otherwise lead relatively normal intellectual, personal, and social lives.
Turner syndrome (XO) is the absence of, or an imperfect, second X chromosome. Turner syndrome leads to ovarian regression either impairing or eliminating the production of ovarian hormones. Turner syndrome occurs in 1 of every 2500 live births of individuals identified as female at birth and affects the individual’s cognitive functioning and sexual maturation (Lally & Valentine-French, 2019). The external genitalia appear normal, but breasts and ovaries do not develop fully and the individual typically does not menstruate, causing infertility. Turner syndrome also results in a short stature and other physical characteristics. During development, those with Turner syndrome exhibit reduced performance on tasks at which females excel and males excel, while sex-neutral tasks are not affected (Hines, 2011).
Triple X syndrome (XXX) is the presence of an additional X chromosome in the cells of a female and occurs in 1 out of 1000 female births. Other than being taller than average, there are no unusual physical features associated with Triple X syndrome. Sexual development and conception rates are normal, however there is an increased risk of delays in learning, motor skills, and speech and language development. In approximately 10% of females with Triple X syndrome, seizures or kidney abnormalities occur (National Institutes of Health, 2020).
Klinefelter syndrome (XXY) results when an extra X chromosome is present in the cells of a male and occurs in 1 out of 650 male births. The Y chromosome stimulates the growth of male genitalia, but the additional X chromosome inhibits this development. An individual with Klinefelter syndrome typically has small testes, some breast development, infertility and low levels of testosterone. Additionally, motor delays and learning disabilities are often present (National Institutes of Health, 2019).
Jacob’s syndrome (XYY) results when an extra Y chromosome is present in the cells of a male and occurs in 1 out of 1000 male births. Males with this condition tend to be taller than average, and a large head, large teeth, flat feet, widely spaced eyes, and scoliosis have also been noted in some males. While normal testosterone production and sexual development occur , Jacob’s syndrome is associated with an increased risk of learning disabilities and delayed speech, language, and motor skills. An increased risk of motor tics, seizures, asthma, attention-deficit/ hyperactivity disorder, depression, and autism spectrum disorder occur (National Institutes of Health, 2020).
Androgen Insensitivity Syndrome (AIS) occurs when a person has one X and one Y chromosome, but is resistant to the male hormones or androgens. Individuals with AIS lack the receptors that enable androgens to activate genes in the cell’s nucleus. This results in the partial or complete inability of the cell to respond to androgens and affects approximately 1 in 20,000 XY individuals (Carroll, 2016). Because the Wolffian ducts do not respond to the testosterone, male genitalia do not develop. Because the gonads did produce the Mullerian inhibiting substance, the Mullerien ducts do not develop into normal female internal organs. Consequently, the individual appears to be female at birth, but has an XY chromosomal pattern. It is often not until puberty, when there is a lack of menstruation due to the missing ovaries and other internal reproductive systems, that AIS is detected (Hines, 2015)..
Partial Androgen Insensitivity syndrome (PAIS) and mild forms of androgen insensitivity syndrome result when the body’s tissues are partially sensitive to the effects of androgens (National Institutes of Health, 2020). Individuals with partial androgen insensitivity can have genitalia that look typically female, typically male, or have both male and female characteristics. Individuals with mild androgen insensitivity are born with male sex characteristics, but are often infertile and experience breast enlargement at puberty.
Congenital Adrenal Hyperplasia (CAH) is a group of genetic disorders which cause increased production of androgens due to an enzymatic deficiency (21-hydroxylase) resulting in an inability to produce cortisol and the overproduction of androgens (Hines, 2015). CAH occurs in between 1/5000 and 1/20,000 births in the United States and Europe. High androgen levels are expected in embryos with an XY pattern. For those embryos with an XX-pattern, however, an increase in androgens results in females exhibiting an increase in male-typical play and reduced female-typical play. Also, women who took an androgenic progestin, that mimics androgen, during pregnancy have children who exhibit an increase in male-typical toys and activities, while women who took antiandrogenic progestins, that mimic progesterone, show a decreased interest in male-typical activities and toys. Additionally, females with CAH show greater levels of physical aggression, increased accuracy in throwing objects at targets, and some studies have indicated enhanced mental rotation abilities (Hines, 2011).
Convincing evidence indicates that both prenatal and postnatal exposure to testosterone influences the development of children’s sex typical toy and activity interests. For example, boys prefer toys that move and “prenatal androgen exposure may increase interest in watching things move in space by altering development of the visual system,” (Hines, 2011, p. 74). Additionally, boys spend more time in “rough and tumble” play and prefer cars over dolls. For females, higher levels of testosterone in the blood and amniotic fluid in pregnant women, was correlated with higher levels of male typical play behavior and reduced female typical play behavior in their daughters (Hines, 2015).
Puberty
Puberty is a period of rapid growth and sexual maturation. These changes begin sometime between eight and fourteen. Girls begin puberty at around ten years of age and boys begin approximately two years later. Pubertal changes take around three to four years to complete. Adolescents experience an overall physical growth spurt first. Sexual changes that occur at puberty are divided into two categories: Primary sexual characteristics and secondary sexual characteristics.
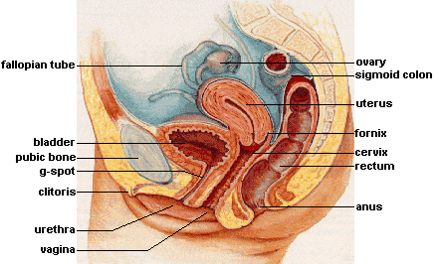
Primary sexual characteristics are changes in the reproductive organs. For males, this includes growth of the testes, penis, scrotum, and spermarche or first ejaculation of semen. This occurs between 11 and 15 years of age. For females, primary characteristics include growth of the uterus and menarche or the first menstrual period. The female gametes, which are stored in the ovaries, are present at birth, but are immature. Each ovary contains about 400,000 gametes, but only 500 will become mature eggs (Crooks & Baur, 2007). Beginning at puberty, one ovum ripens and is released about every 28 days during the menstrual cycle. Stress and higher percentage of body fat can bring menstruation at younger ages.
Female Reproductive System
Male Reproductive System

 Secondary sexual characteristics are visible physical changes not directly linked to reproduction, but signal sexual maturity. For males this includes broader shoulders and a lower voice as the larynx grows. Hair becomes coarser and darker, and hair growth occurs in the pubic area, under the arms and on the face. For females breast development occurs around age 10, although full development takes several years. Hips broaden and pubic and underarm hair develops and also becomes darker and coarser.
Secondary sexual characteristics are visible physical changes not directly linked to reproduction, but signal sexual maturity. For males this includes broader shoulders and a lower voice as the larynx grows. Hair becomes coarser and darker, and hair growth occurs in the pubic area, under the arms and on the face. For females breast development occurs around age 10, although full development takes several years. Hips broaden and pubic and underarm hair develops and also becomes darker and coarser.
Not surprisingly, puberty has a tremendous affect on gender identity. For cisgender adolescents, males typically welcome the physical transition as their bodily changes represent the masculine ideal, especially regarding increased muscularity. In contrast, the physical changes experienced by females often take them further away from the feminine ideal of being very thin. Additionally, girls who develop earlier than their peers tend to be sexualized and harassed for their development.
Gender Role Intensification: At about the same time that puberty accentuates gender identity, role differences also accentuate for at least some teenagers. Some girls who excelled at math or science in elementary school, may curb their enthusiasm and displays of success at these subjects for fear of limiting their popularity or attractiveness as girls (Taylor et al., 1995; Sadker, 2004). Some boys who were not especially interested in sports previously may begin dedicating themselves to athletics to affirm their masculinity in the eyes of others. For trans adolescents, puberty can be especially difficult if the physical changes experienced do not align with the adolescents’ gender identification. These changes can cause distress in the adolescent, especially if trans-affirmative care is not being provided.
Pubertal Blockers and Hormone Treatment: Increasingly, transgender children, or those who identify with a gender that is different than the one assigned at birth, are socially transitioning to reflect their gender identity. This includes changing names, pronouns, clothing, hairstyles, and peer groups. Needless to say, the changes that occur during puberty can cause significant distress for transgender and gender nonconforming children and adolescents. Consequently, pubertal blockers or medications that suppress puberty by halting the production of estrogen or testosterone, have been prescribed to peripubertal transgender youth. The medications mostly commonly used to suppress puberty are known as gonadotropin-releasing hormone (GnRH) analogues (Mayo Clinic, 2022). When taken regularly, GnRH analogues suppress the body’s release of sex hormones during puberty by desensitizing the stimulatory effects of GnRH on the pituitary gland, which secretes reproductive hormones. In those identified as male at birth, GnRH analogues decrease the growth of facial and body hair, prevent voice deepening, and limit the growth of genitalia. In those identified as female at birth, treatment limits or stops breast development and stops menstruation. The medications may be given as shots in a doctor’s office every one, three or six months, or in a yearly implant (Wilson, 2021).
By temporarily pausing development, the use of GnRH analogues allows preadolescents more opportunity to further explore and confirm their gender identity before the use of other treatments. Pubertal blockers are associated with improved behavioral and emotional functioning in transgender youth, including decreased rates of depression and suicidal ideation (Roberts, 2022). When puberty blockers are initiated in the early stages of puberty, physicians suggest that patients stop using them by age 14 (Wilson, 2021). At that point, patients, parents and physicians need to decide whether to introduce hormones that align with their gender identity, or resume puberty in the gender assigned at birth.
Because gender-affirming hormone treatment, which aligns one’s physical body with their gender identification, results in fertility and appearance changes, adolescents should understand the implications of the treatments. According to Roberts (2022), by age 16 adolescents are considered to possess the mental capacity to understand the hormonal effects and provide informed consent. Gender-affirming hormone treatment, has also been shown to increase mental health functioning among transgender youth.
Female Sexual and Reproductive Health at Midlife
The climacteric, or the midlife transition when fertility declines, is biologically based but impacted by the environment. Women, however, lose their ability to reproduce once they reach menopause. Perimenopause refers to a period of transition in which a woman’s ovaries stop releasing eggs and the level of estrogen and progesterone production decreases. Menopause is defined as 12 months without menstruation. The average age of menopause is approximately 51, however, many women begin experiencing symptoms in their 40s. These symptoms occur during perimenopause, which can occur 2 to 8 years before menopause (Huang, 2007). A woman may first begin to notice that her periods are more or less frequent than before. After a year without menstruation, a woman is considered menopausal and no longer capable of reproduction.
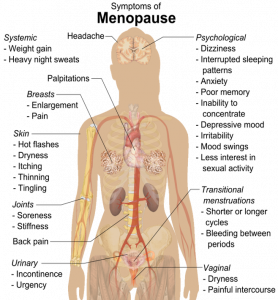 Symptoms: The symptoms that occur during perimenopause and menopause are typically caused by the decreased production of estrogen and progesterone (North American Menopause Society, 2016). The shifting hormones can contribute to the inability to fall asleep. Additionally, the declining levels of estrogen may make a woman more susceptible to environmental factors and stressors which disrupt sleep. A hot flash is a surge of adrenaline that can awaken the brain from sleep. It often produces sweat and a change of temperature that can be disruptive to sleep and comfort levels. Unfortunately, it may take time for adrenaline to recede and allow sleep to occur again (National Sleep Foundation, 2016).
Symptoms: The symptoms that occur during perimenopause and menopause are typically caused by the decreased production of estrogen and progesterone (North American Menopause Society, 2016). The shifting hormones can contribute to the inability to fall asleep. Additionally, the declining levels of estrogen may make a woman more susceptible to environmental factors and stressors which disrupt sleep. A hot flash is a surge of adrenaline that can awaken the brain from sleep. It often produces sweat and a change of temperature that can be disruptive to sleep and comfort levels. Unfortunately, it may take time for adrenaline to recede and allow sleep to occur again (National Sleep Foundation, 2016).
The loss of estrogen also affects vaginal lubrication which diminishes and becomes waterier and can contribute to pain during intercourse. The vaginal wall also becomes thinner, and less elastic. Estrogen is also important for bone formation and growth, and decreased estrogen can cause osteoporosis resulting in decreased bone mass. Depression, irritability, and weight gain have been blamed on menopause, but they are not menopausal (Avis et al., 2001; Rossi, 2004). Weight gain can occur due to an increase in intra-abdominal fat followed by a loss of lean body mass after menopause (Morita et al., 2006). Consequently, women may need to change their lifestyle to counter any weight gain. Depression and mood swings are more common during menopause in women who have prior histories of these conditions rather than those who have not. Additionally, the incidence of depression and mood swings is not greater among menopausal women than non-menopausal women. Women vary greatly in the extent to which these symptoms are experienced. Most American women go through menopause with few problems (Carroll, 2016). Overall, menopause is not seen as universally distressing (Lachman, 2004).
Hormone Replacement Therapy: Concerns about the effects of hormone replacement has changed the frequency with which estrogen replacement and hormone replacement therapies have been prescribed for menopausal women. Estrogen replacement therapy was once commonly used to treat menopausal symptoms. However, more recently, hormone replacement therapy has been associated with breast cancer, stroke, and the development of blood clots (NIH, 2007). Most women do not have symptoms severe enough to warrant estrogen or hormone replacement therapy. If so, they can be treated with lower doses of estrogen and monitored with more frequent breast and pelvic exams. There are also some other ways to reduce symptoms. These include avoiding caffeine and alcohol, eating soy, remaining sexually active, practicing relaxation techniques, and using water-based lubricants during intercourse.
Menopause and Ethnicity: In a review of studies that mentioned menopause, symptoms varied greatly across countries, geographic regions, and even across ethnic groups within the same region (Palacios et al., 2010). For example, the Study of Women’s Health across the Nation (SWAN) examined 14,906 white, African American, Hispanic, Japanese American, and Chinese American women’s menopausal experiences (Avis et al., 2001). After controlling for age, educational level, general health status, and economic stressors, white women were more likely to disclose symptoms of depression, irritability, forgetfulness, and headaches compared to women in the other racial/ethnic groups. African American women experienced more night sweats, but this varied across research sites. Finally, Chinese American and Japanese American reported fewer menopausal symptoms when compared to the women in the other groups. Overall, the Chinese and Japanese group reported the fewest symptoms, while white women reported more mental health symptoms and African American women reported more physical symptoms.
Cultural Differences: Cultural influences seem to also play a role in the way menopause is experienced. Further, the prevalence of language specific to menopause is an important indicator of the occurrence of menopausal symptoms in a culture. Hmong tribal women living in Australia and Mayan women report that there is no word for “hot flashes” and both groups did not experience these symptoms (Yick-Flanagan, 2013). When asked about physical changes during menopause, the Hmong women reported lighter or no periods. They also reported no emotional symptoms and found the concept of emotional difficulties caused by menopause amusing (Thurston & Vissandjee, 2005). Similarly, a study with First Nation women in Canada found there was no single word for “menopause” in the Oji-Cree or Ojibway languages, with women referring to menopause only as “that time when periods stop” (Madden et al., 2010).
While some women focus on menopause as a loss of youth, womanhood, and physical attractiveness, career-oriented women tend to think of menopause as a liberating experience. Japanese women perceive menopause as a transition from motherhood to a more whole person, and they no longer feel obligated to fulfill certain expected social roles, such as the duty to be a mother (Kagawa-Singer et al., 2002). In India, 94% of women said they welcomed menopause. Aging women gain status and prestige and no longer have to go through self-imposed menstrual restrictions, which may contribute to Indian women’s experiences (Kaur et al., 2004). Overall, menopause signifies many different things to women around the world and there is no typical experience. Further, normalizing rather than pathologizing menopause is supported by research and women’s experiences.
Male Sexual and Reproductive Health at Midlife
During midlife, men may experience a reduction in their ability to reproduce. Although males can continue to father children throughout middle adulthood, erectile dysfunction (ED) becomes more common. Erectile dysfunction refers to the inability to achieve an erection or an inconsistent ability to achieve an erection (Swierzewski, 2015). Intermittent ED affects as many as 50% of men between the ages of 40 and 70. About 30 million men in the United States experience chronic ED, and the percentages increase with age. Approximately 4% of men in their 40s, 17% of men in their 60s, and 47% of men older than 75 experience chronic ED.
Causes for ED are primarily due to medical conditions, including diabetes, kidney disease, alcoholism, and atherosclerosis (build-up of plaque in the arteries). Plaque is made up of fat, cholesterol, calcium and other substances found in the blood. Over time plaque builds up, hardens, and restricts the blood flow in the arteries (NIH, 2014). This build-up limits the flow of oxygenated blood to organs and the penis. Overall, diseases account for 70% of chronic ED, while psychological factors, such as stress, depression and anxiety account for 10%-20% of all cases. Many of these causes are treatable, and ED is not an inevitable result of aging.
 Men during middle adulthood may also experience prostate enlargement, which can interfere with urination, and deficient testosterone levels which decline throughout adulthood, but especially after age 50. If testosterone levels decline significantly, it is referred to as andropause or late-onset hypogonadism. Identifying whether testosterone levels are low is difficult because individual blood levels vary greatly. Low testosterone is not a concern unless it accompanied by negative symptoms such as low sex drive, ED, fatigue, loss of muscle, loss of body hair, or breast enlargement. Low testosterone is also associated with medical conditions, such as diabetes, obesity, high blood pressure, and testicular cancer. The effectiveness of supplemental testosterone is mixed, and long term testosterone replacement therapy for men can increase the risk of prostate cancer, blood clots, heart attack and stroke (WebMD, 2016). Most men with low testosterone do not have related problems (Berkeley Wellness, 2011).
Men during middle adulthood may also experience prostate enlargement, which can interfere with urination, and deficient testosterone levels which decline throughout adulthood, but especially after age 50. If testosterone levels decline significantly, it is referred to as andropause or late-onset hypogonadism. Identifying whether testosterone levels are low is difficult because individual blood levels vary greatly. Low testosterone is not a concern unless it accompanied by negative symptoms such as low sex drive, ED, fatigue, loss of muscle, loss of body hair, or breast enlargement. Low testosterone is also associated with medical conditions, such as diabetes, obesity, high blood pressure, and testicular cancer. The effectiveness of supplemental testosterone is mixed, and long term testosterone replacement therapy for men can increase the risk of prostate cancer, blood clots, heart attack and stroke (WebMD, 2016). Most men with low testosterone do not have related problems (Berkeley Wellness, 2011).
In the next module we will consider the various theories that have been proposed to explain the development of gender identity. In addition, we will examine the sources of gender socialization.


